Over the years we have hosted more than 25 Slipstream Weekends throughout Canada and the US. We wanted to share some of our insights from our favourite sessions at Slipstream. Stay tuned for guest posts from the experts and highlights from the CIM Team. To kick things off… Diabetes and Nutrition.
CIM hosted the first-ever 5.5er Slipstream weekend in June for adults with Type 1 diabetes and their partners, friends, or family members without diabetes. We were joined by Registered Dietitian, Certified Diabetes Educator, and fellow Type 1 Lorraine Anderson, who shared two diabetes-themed presentations over the weekend. Read on for her recap of the first presentation, Diabetes and Nutrition.
Words by Lorraine Anderson
I was very fortunate to lead a great discussion amongst an enthusiastic group of adults living with Type 1 diabetes, as well as several “5.5ers”, on the role of nutrition and healthy eating in the management of Type 1 diabetes. Below are some of the key takeaways from the presentation on diabetes and nutrition:
Healthy eating recommendations are similar, T1D or not
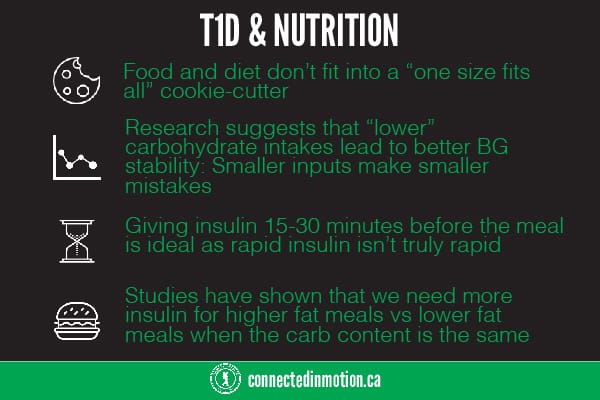
Dietary recommendations for adults with Type 1 diabetes are very similar to the healthy eating guidelines encouraged for all. The best approach to healthy eating for anyone involves working with a dietitian to customize a balance of macronutrients (carbohydrate, protein, and fat) selected from a wide range of nutrient-rich foods. Food and diet don’t fit into a “one size fits all” cookie-cutter – preferences, cultural backgrounds, other medical concerns (i.e. celiac disease, allergies) and personal choices all need to be considered.

Not all carbohydrates are created equally
And not all carbohydrates affect BGs equally. We talked about the “Law of Small Numbers” and some recent research1 suggesting that “lower” carbohydrate intakes do seem to lead to better BG stability. Smaller inputs make smaller mistakes, so it only makes sense that we see less highs and less lows with a lower- to moderate-carb intake (100 to 150g/day). This is a conversation to have with your diabetes team to discuss what dietary strategy will work best for you. We have lots of tools to help us to count carbs but research2 shows that we are often off by 20% and sometimes by even more. In addition, occasionally nutrition labels can be inaccurate3 so it’s no wonder we have so much difficulty keeping post-meal BG’s in range.

Timing is everything
The timing of a meal-time bolus is also very important to help us best match insulin to food. For most meals, giving insulin 15-30 minutes before the meal is ideal as rapid insulin isn’t truly rapid! FIASP® (faster-acting insulin aspart) is a new ultra-rapid insulin that is recommended to be given up to 2 minutes before or up to 20 minutes after the meal. Fiasp® is not approved for use in pumps as of today. Eating protein and vegetables first followed by carbohydrate later in the meal may help improve post-meal BG4. Studies show that increasing the acidity of a meal can lower glycemic response, so it might be helpful to flavour foods with lemon and vinegar, and don’t forget to add a slice of tomato to that sandwich!

To dose or not to dose: High protein and high fat
There was a lot of interest around dosing of insulin for higher-protein and higher-fat meals. One of the methods discussed was the use of Fat Protein Units (FPU’s). This formula was developed in Europe and suggests that 100 calories of fat or protein can have a “carb equivalent” effect of approximately 10g of carb. However, the impact of protein and fat on BG is greatly delayed compared to the impact of carbohydrate, so for those using insulin pumps the usual direction is to bolus for the carb portion of the meal NOW and give an extended/dual wave bolus for the fat/protein effect seen later. The more fat/protein in the meal, the larger and the longer the extended bolus. 1 FPU is extended over 3 hours, 2 FPU over 4 hours, 3 FPU over 5 hours and >3 FPU’s are recommended to be extended over 8 hours. Fortunately, there are exchange lists available that tell you how many FPU’s are in various foods, so you don’t need to be a walking calculator (any more than you already are!). Fat slows the rate at which our stomachs empty and can make us resistant to the insulin we take. Studies have shown that we need more insulin for higher fat meals vs lower fat meals when the carb content is the same5. Paying attention to dietary fat is important when striving for tight diabetes control. Fat and protein increase post meal BG’s and the effect has been found to be additive6. Protein has different effects when consumed with and without carb (i.e. 30g of protein with carb will affect BG vs. ≥ 75g protein without carb). Pumpers have the advantage of using a temp basal increase or extending bolus delivery to match the effect of higher fat/protein meals.
For MDI users, a bolus for higher fat meals can be split by giving the insulin dose, calculated for the meal using your I:C (insulin to carbohydrate) ratio, before the meal and then giving an additional 30% of that dose 3 hours after the meal7. In a small study, this approach has been found to produce a post-meal CGM graph like what is seen when a low-fat meal is consumed. In real life, eating out presents numerous challenges for many people living with Type 1 diabetes, even when detailed nutrition information is readily available. Looking at the carb content of restaurant meals is important but don’t forget to check how much fat and protein are in menu items. This might be one of the reasons why we often see BG struggles after eating out.
Please consult your individual diabetes care team before making any changes to your insulin doses. The studies that were referenced are listed below, however they cannot be generalized to everyone. Diabetes is unique to each of us and it is important that you discuss your care plan with health care professionals who know you and your diabetes.
1. Lennerz et al. Pediatrics. 2018. 141 (60); e20173349.
2. Brazeau et al. Diab Res Clin Prac. 2013; 99: 19-23.
3. Smart et al. Nutr Dietet. 2011. 68: 227-230.
4. Shukla, AP et al. Diabetes Care. 2015; 38(7): e98-e99.
5. Wolpert et al. Diabetes Care. April 2013; 36: 810
7. Campbell, M et al. Diabetes Care 2016; 39: e141-e142.
Disclaimer: Although this is not paid content, Lorraine’s time was paid for by our partners at One Touch. OneTouch is one of the national partners of Connected in Motion. Our views may be biased because of these partnerships, but we still thought this information was helpful for the community.