Words by Amanda Coschi | Photos by Blair Ryan
In August a group of 13 individuals came together to complete one of Canada’s most difficult hikes, the North Coast Trail (NCT). If there is one thing I learned about the trail, it is that it had a sense of humor – much like diabetes! Looking back, I find myself thinking about how our group managed to conquer both the unpredictability and challenges of the trail and the unpredictability and challenges of diabetes. Part of the answer is in looking at the numbers, but we must also look past them to see the bigger picture.
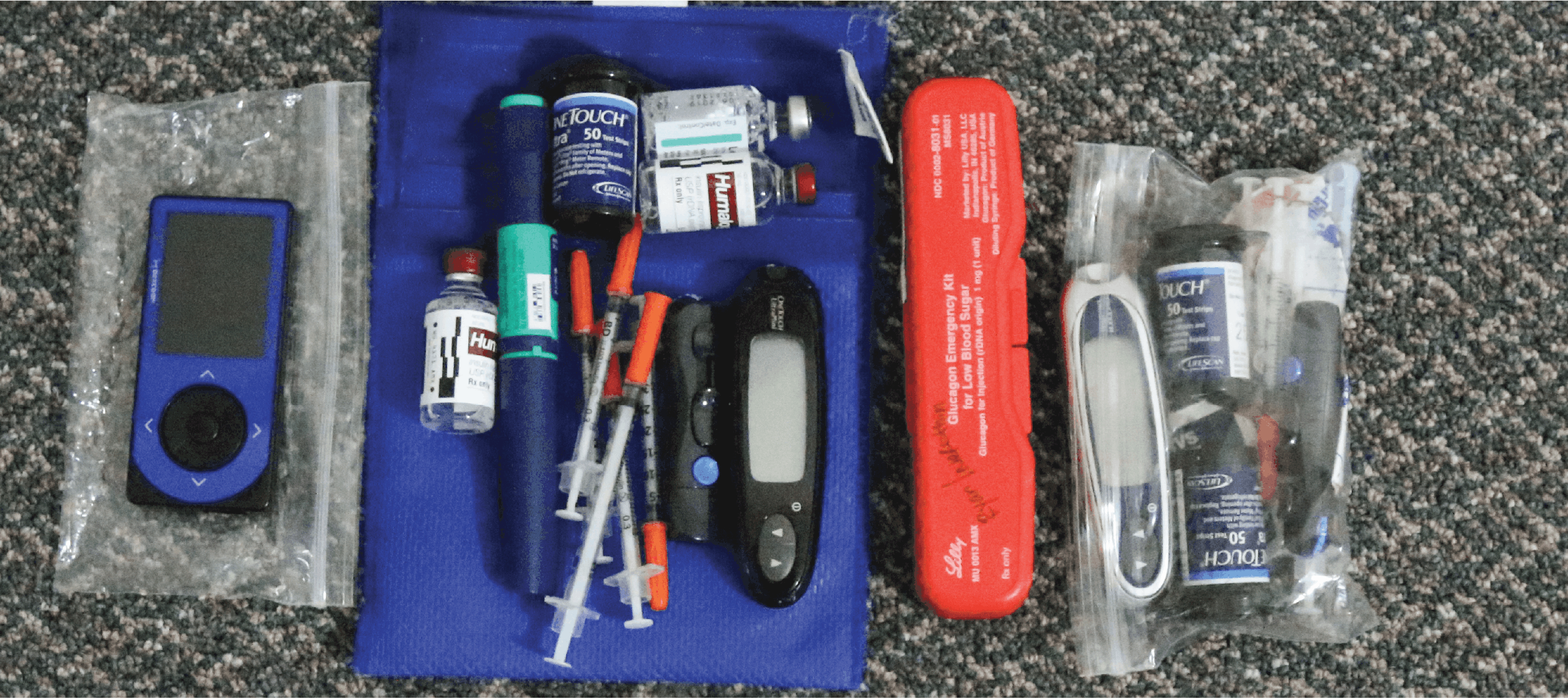
A short background about myself: I was diagnosed with Type 1 diabetes in 2002 and have since spent my summers at diabetes camp in some way shape or form. I have become more and more actively involved with the Connected in Motion community over the years, and this recently led me to become 1 of the 13 members on the NCT hike. I completed my Bachelor of Science in Nursing in 2014 and have been working as a Registered Nurse in Paediatrics/NICU. I am a Certified Diabetes Educator and also do pump training and education with Animas Canada. I’m writing today to share my experiences and viewpoints of managing diabetes on the North Coast Trail. This should not be taken as strict medical advice, but rather the hope is you may read something useful to add to your diabetes toolkit.
Managing Type 1 diabetes often comes down to the numbers: what is our sugar level, what are our ratios, what are our rates, what are our total daily doses, how many carbs in this meal, what is our A1C? There are formulas and equations, and algorithms all meant to try and make diabetes a black and white scenario: carbohydrates make your blood glucose go up, insulin makes your blood glucose go down. Makes sense, right? However, we all know that diabetes has so many shades of grey that it would make even the most fictional of characters blush. So when it came to the NCT, I had to quickly wrap my head around the fact that the numbers weren’t always going to follow textbook guidelines. When providing diabetes education to individuals and families, I often remind them that diabetes is, unfortunately, a guessing game of trial and error. There are guidelines and recommendations, but the only guideline that matters is whether or not it worked for you. More often than not, we have to make adjustments and try again.

To put it into perspective…
My basal rates add up to a daily total of approximately 15u which actually fits quite nicely into some of the guidelines and formulas out there based on my weight and total daily dose. On the NCT I went to a total of 4.8u of basal a day. To break that down, while hiking my basal ran at a rate of 0.1u/hr. It took me a while to trust that this unnervingly small amount of insulin was working for me. However, if everyone had done a 70% basal decrease we would have had blood sugar readings all over the map.
Recommendation and rational…
Typically, a standard temporary basal rate reduction for moderate exercise is -50% at least one hour before the start of exercise. Injectors may need to decrease their long acting insulin dose in advance if the exercise is planned ahead. The best way to figure it out however, is trial and error. I ran a lot of temporary basals before discovering the rate that worked for me. Our group had a wide range of athletes: marathon runners, iron man competitors, amazing cyclists, semi-pro soccer and hockey players, and individuals like me who were reasonably fit with a love for the outdoors. A blanket statement for insulin adjustments would have never worked for our group. There are too many factors to discuss here, but everything from the type of exercise, duration of exercise, and level of fitness can impact these recommendations. The goal is to achieve a blood insulin level that is high enough to prevent your sugar from rising, but low enough to allow your muscles access to internal energy stores (1). Essentially, you must try to mimic what the body does perfectly…simple, right?

To put it into perspective…
The other number people living with diabetes must constantly remember is carbohydrates. Our group packed A LOT of food. We joked with other hikers that we had food anxiety when they saw how much we packed. We were spoiled with exceptional freeze-dried meals provided by Briden Solutions, and also sponsored by Clif Bars that provided a delicious and necessary snack along the trail. To give you an idea of how much we were eating, I was at 3 bars by the end of day 1; we were burning 500-700 calories an hour on the trail! One of the members even had a video blog keeping track of what number of bar he was on! Much like my basal, it took time to get used to how little insulin I needed at meals, as well as the fact that I didn’t need to take any insulin at all for a 40g Clif Bar.
Recommendation and rational…
Once again managing diabetes is about finding what works for you. When hiking the beach terrain, even though it was challenging, I found a reduction in basal and lower boluses at meals was sufficient to keep my sugars in range. As soon as we came to an incline that was so steep it required a rope to climb, my continuous glucose monitor (CGM) would alert me that my blood sugar was falling too quickly. I learned that it was necessary to eat a Clif bar before any of these challenging areas as I needed the extra carbohydrates to counteract the exertion for this difficult section of terrain. There are many recommendations and guidelines to assist in adjusting carbs to exercise, a blanket statement being 10-15g for 1 hour of moderate intensity activity, and 30-60g for 1 hour of intense exercise (2). I would highly recommend reading John Walsh’s book, Pumping Insulin (2013), who has an excellent and in-depth chapter on exercise.

To put it into perspective…some final recommendations and rational
So what did I learn about managing Type 1 diabetes from this experience? How can I apply what the NCT taught me into my own teaching? The lesson seems to be that numbers are important, but they are only a starting point of diabetes management. You can make as many calculations as you want, but then you need to figure out if it actually works for you, and if it doesn’t work, make adjustments and try again! On top of that, I want to remind you that diabetes management can be unpredictable – just like the NCT! Don’t be upset if you think that you’ve found the solution, and then the next day it doesn’t work. As mentioned, diabetes has a sense of humor. We can never fully know what to expect, despite the fact that two days may appear to have an identical routine. It’s so easy to get wrapped up in the numbers, as they’re a large part of living with diabetes. However, hiking the NCT taught me that numbers can be misleading! One day we hiked 7km in 7hrs. The next day we pushed through 18km in 7hrs! It was unpredictable, and it all depended on the terrain that day.
So here’s the big take away: 13 incredible individuals conquered the NCT and diabetes was never once considered a barrier. In the long run, a high glucose on the trail is quickly forgotten but the memories last forever. None of the hikers would claim to have perfect control. There’s no such thing as perfect, especially with diabetes, so it is important to take a look at the bigger picture! If you’re happy and healthy, don’t let a bump in the road throw you off the track. Take a step back from those frustrating numbers and look at how you are doing overall. Look at everything that you’ve accomplished despite the challenges diabetes throws your way every day. I will always be proud of myself for completing the NCT, and I can tell you that I’ve already forgotten what my sugars were like. All I can promise you is that they weren’t perfect.
Happy hiking!

Sources:
(1) Walsh, J., & Roberts, R. (2013). Pumping insulin: everything you need to succeed on an insulin pump(5th ed.). San Diego: Torrey Pines Press.
(2) Building competency in diabetes education: the essentials(4th ed.). (2013). Toronto, ON: Diabetes Educator Section, Canadian Diabetes Association.
About Amanda Coschi
 Amanda was diagnosed with Type 1 diabetes at age 10 and since then her diabetes has been taking her on wild adventures! Amanda grew up in Aurora, ON but spent her summers in Huntsville at Camp Huronda where she learned of her love for canoe trips and the outdoors. She spent many summers as a camper and after completion of her Bachelor’s of Science in Nursing at McMaster University and obtaining her Certified Diabetes Educator she continued her summers at camp this time attending the canoe trips as their nurse. In the winter you can find her with a pair of skates, skis or her snowboard on her feet. Amanda is beyond excited for this opportunity to start another adventure and give back to an organization that has been an invaluable support network for her!
Amanda was diagnosed with Type 1 diabetes at age 10 and since then her diabetes has been taking her on wild adventures! Amanda grew up in Aurora, ON but spent her summers in Huntsville at Camp Huronda where she learned of her love for canoe trips and the outdoors. She spent many summers as a camper and after completion of her Bachelor’s of Science in Nursing at McMaster University and obtaining her Certified Diabetes Educator she continued her summers at camp this time attending the canoe trips as their nurse. In the winter you can find her with a pair of skates, skis or her snowboard on her feet. Amanda is beyond excited for this opportunity to start another adventure and give back to an organization that has been an invaluable support network for her!