For those of us living with diabetes, we know that types 1 and 2 often get confused. But did you know that there are at least 6 other types of diabetes as well? In honor of Diabetes Awareness Month, we’re taking a look at the many different types of diabetes. Keep reading to learn more about how varied this chronic illness really is!
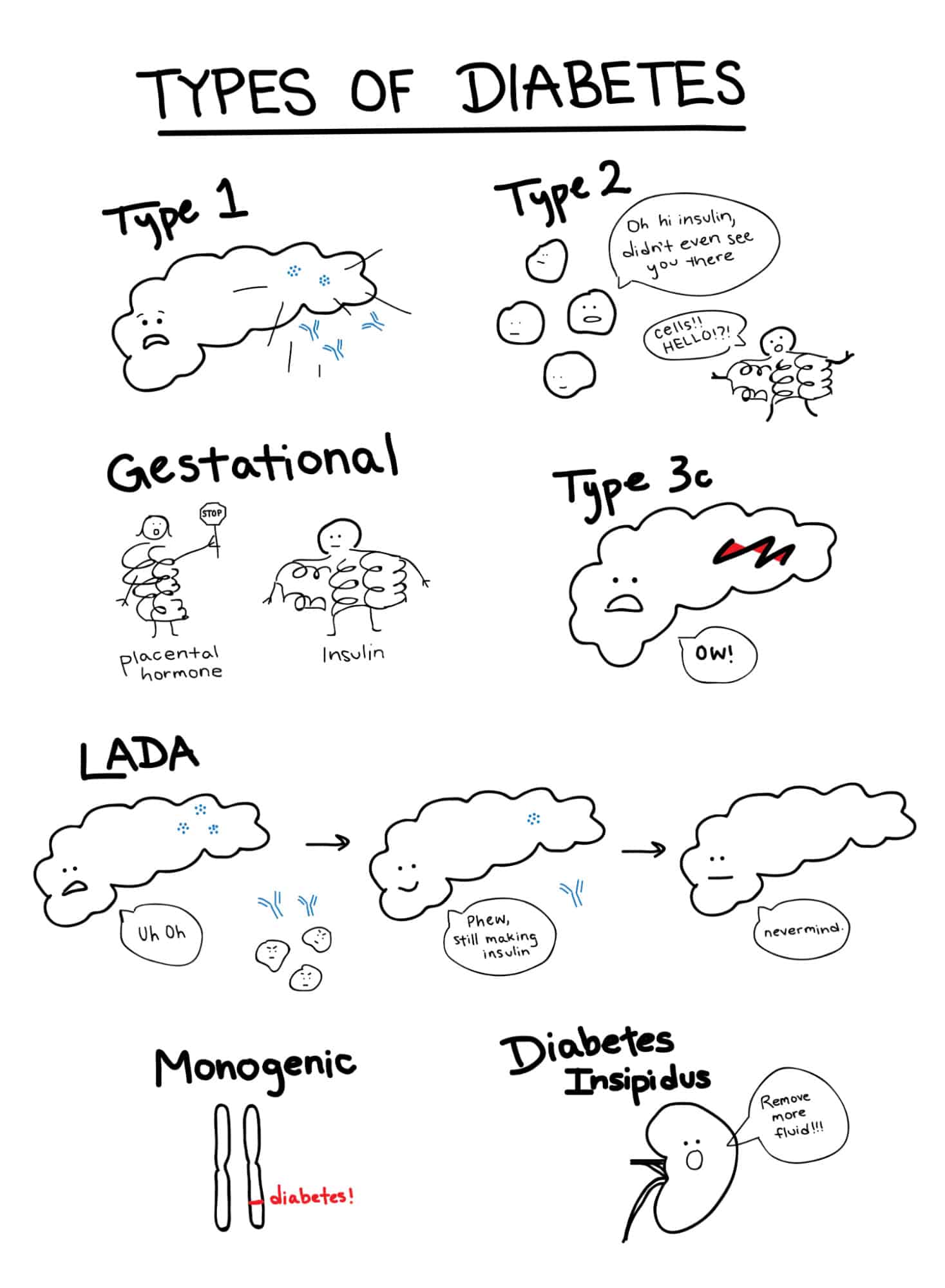
Type 1 Diabetes

If you’re reading this blog, you’re probably pretty familiar with T1D 🙂 I’ll just give a quick overview for good measure.
Type 1 diabetes mellitus is an autoimmune disease in which the immune system mistakenly attacks the insulin-producing beta cells of the pancreas. Without insulin, the body can’t let glucose in the blood enter cells and be converted to energy. It’s unclear what causes the onset of type 1, but it’s thought to be some combination of genetic factors and environmental factors such as viral infection. Typical symptoms include frequent urination, excessive thirst, weight loss, and fatigue. Type 1 diabetes is managed with BG monitoring and insulin therapy. Approximately 5-10% of people with diabetes have type 1 [1].
Type 2 Diabetes
While type 1 diabetes is caused by a lack of insulin, type 2 diabetes mellitus is caused by resistance to insulin. That basically means that cells stop responding to insulin how they usually would. Like type 1, type 2 diabetes is also caused by a combination of genetic and environmental factors. Having a family history of type 2 diabetes, being overweight, and being inactive can be risk factors [2]. Management strategies for type 2 diabetes can include diet, exercise, medication, BG monitoring, and insulin therapy [3]. Type 2 is the most common form of diabetes; it has been estimated that 90% of diabetes cases among Canadian adults are type 2 [4]. If you’re looking for more resources on type 2 diabetes, check out Beyond Type 2.

Gestational Diabetes

Gestational diabetes is diagnosed for the first time during pregnancy and it usually develops in the middle of gestation [5]. Hormones released by the placenta during pregnancy can block the action of insulin and increase the body’s insulin needs. Sometimes the pregnant person cannot produce and/or use enough insulin and develops insulin resistance [6, 7]. Gestational diabetes can be managed with diet, exercise, BG monitoring, and sometimes insulin therapy. Gestational diabetes usually goes away after delivery, but it can increase the risk of developing type 2 diabetes later in life [8]. Gestational diabetes is reported in approximately 5.5% of births in Canada [4].
Type 3c Diabetes
Type 3c diabetes, also referred to as pancreatogenic diabetes, occurs from damage to the pancreas. Examples include chronic pancreatitis-associated diabetes and cystic fibrosis-related diabetes. Prolonged inflammation in the former and scarring from mucus buildup in the latter can cause insulin deficiency [9]. Pancreatic cancer and surgical removal of the pancreas can also lead to type 3c diabetes. Because there is limited awareness of and insurance coverage for type 3c diabetes, it often goes misdiagnosed.
While the pancreas’ important role in insulin production usually gets most of the attention, that little organ is multifaceted–it’s got a lot of jobs! In terms of endocrine function, it releases quite a few other hormones to regulate carbohydrate metabolism including glucagon, somatostatin, pancreatic polypeptide, and amylin. In terms of exocrine function, it also releases digestive enzymes. Thus, people with type 3c diabetes can also experience the effects of these additional pancreatic functions being inhibited [10]. For example, people with type 3c diabetes may also need to take digestive enzyme supplements [10].

Latent Autoimmune Diabetes in Adults (LADA)

Like type 1 diabetes, LADA is an autoimmune condition that occurs when the immune system attacks insulin-producing cells in the pancreas. In contrast to type 1 diabetes, however, LADA progresses slowly and usually occurs in adults over the age of 30 [11]. Because people with LADA often still produce some insulin for months or years after they are diagnosed, it is frequently misdiagnosed as type 2 diabetes [11]. Low C-peptide levels and high levels of antibodies against pancreatic islets can help distinguish LADA from type 2 diabetes [12]. LADA is sometimes called type 1.5 diabetes because it shares characteristics with both types 1 and 2. Some researchers believe LADA is varied and can exist on a diabetes continuum of sorts between types 1 and 2 [11, 12]. At first, LADA can often be managed with diet, exercise, and potentially medication, but it eventually requires insulin therapy [11]. It is estimated that LADA may account for 2 – 12% of all cases of diabetes in adults [12].
Monogenic Diabetes
While other types of diabetes are caused by multiple genes in addition to environmental factors, monogenic diabetes is caused by a genetic mutation in a single gene [13]. Examples of monogenic diabetes include Maturity Onset Diabetes of the Young (MODY) and Neonatal diabetes [14]. MODY is usually diagnosed in adolescence or early adulthood [13]. It can be caused by numerous mutations including ones in the HNF1-alpha gene, the HNF1-beta gene, and the glucokinase gene [14]. As a result, different types of MODY have different manifestations and require different treatments which can include diet, exercise, insulin therapy, and sulfonylureas [14]. Neonatal diabetes, on the other hand, is usually diagnosed in infants and can be treated with sulfonylurea agents [14].
Monogenic diabetes is often misdiagnosed: for example, MODY can be mistaken for type 2 diabetes when detected in adulthood and neonatal diabetes can be mistaken for type 1 [13]. People with monogenic diabetes usually have a strong family history of diabetes (though mutations can also occur spontaneously), and negative or low levels of antibodies that indicate type 1 diabetes [14]. Diagnosis of monogenic diabetes usually includes a genetic test [14]. It is estimated that 1-2% of all cases of diabetes are monogenic [15].

Diabetes Insipidus

Despite having the word diabetes in it, diabetes insipidus doesn’t have anything to do with the pancreas, insulin, or BG regulation! Diabetes insipidus is when the kidneys pass a large volume of liquid that is dilute and odorless [16]. It occurs when there are problems with the hormone vasopressin aka antidiuretic hormone [17]. Diabetes insipidus shares the name with diabetes mellitus because of common symptoms–both can cause frequent urination and excessive thirst [16]. Like diabetes mellitus, there are different types of diabetes insipidus with different causes and treatments–namely central, nephrogenic, dipsogenic, and gestational [16].
References
[1] “What Is Type 1 Diabetes?” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 25 Mar. 2021, www.cdc.gov/diabetes/basics/what-is-type-1-diabetes.html.
[2] “Insulin Resistance and Diabetes.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 12 Aug. 2019, www.cdc.gov/diabetes/basics/insulin-resistance.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fdiabetes%2Flibrary%2Fspotlights%2Fdiabetes-insulin-resistance.html.
[3] “Type 2 Diabetes.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 20 Jan. 2021, www.mayoclinic.org/diseases-conditions/type-2-diabetes/diagnosis-treatment/drc-20351199.
[4] Canada, Public Health Agency of. “Diabetes in Canada, Highlights from the Canadian Chronic Disease Surveillance System.” Canada.ca, / Gouvernement Du Canada, 17 Aug. 2020, www.canada.ca/en/public-health/services/publications/diseases-conditions/diabetes-canada-highlights-chronic-disease-surveillance-system.html.
[5] “Gestational Diabetes.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 26 Aug. 2020, www.mayoclinic.org/diseases-conditions/gestational-diabetes/symptoms-causes/syc-20355339#:~:text=Gestational%20diabetes%20is%20diabetes%20diagnosed,pregnancy%20and%20your%20baby%27s%20health.
[6] “Gestational Diabetes Mellitus (GDM).” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/gestational-diabetes.
[7] “Gestational Diabetes.” Gestational Diabetes – Symptoms, Treatments | ADA, www.diabetes.org/diabetes/gestational-diabetes.
[8] “Gestational Diabetes and Pregnancy.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 14 July 2020, www.cdc.gov/pregnancy/diabetes-gestational.html.
[9] “Forms Of Diabetes.” Beyond Type 1, 5 July 2020, beyondtype1.org/other-forms-of-diabetes/.
[10] M., Jen. “What I Wish People Knew About Type 3c Diabetes.” Beyond Type 1, 10 Sept. 2020, beyondtype1.org/what-i-wish-people-knew-about-type-3c-diabetes/.
[11] “Latent Autoimmune Diabetes in Adults (LADA): What Is It?” Mayo Clinic, Mayo Foundation for Medical Education and Research, 23 Feb. 2021, www.mayoclinic.org/diseases-conditions/type-1-diabetes/expert-answers/lada-diabetes/faq-20057880#:~:text=Latent%20autoimmune%20diabetes%20in%20adults%20(LADA)%20is%20a%20slow%2D,producing%20cells%20in%20the%20pancreas.
[12] “What Is LADA?” Beyond Type 1, 26 Apr. 2021, beyondtype1.org/what-is-lada-diabetes/.
[13] Monogenic Diabetes (Neonatal Diabetes Mellitus & MODY).” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/monogenic-neonatal-mellitus-mody.
[14] “What Is Monogenic Diabetes?” Beyond Type 1, 29 Jan. 2020, beyondtype1.org/what-is-monogenic-diabetes/.
[15] Lachance, Carl-Hugo. “Practical Aspects of Monogenic Diabetes: A Clinical Point of View.” Canadian Journal of Diabetes, vol. 40, no. 5, 2016, pp. 368–375., doi:10.1016/j.jcjd.2015.11.004.
[16] “Diabetes Insipidus.” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, www.niddk.nih.gov/health-information/kidney-disease/diabetes-insipidus.
[17] Overview, Diabetes Insipidus, NHS, www.nhs.uk/conditions/diabetes-insipidus/#:~:text=Diabetes%20insipidus%20is%20a%20rare,%2C%20even%20at%20night%20(polyuria).